In the healthcare industry, the terms Electronic Health Record (EHR) and Electronic Medical Record (EMR) are often used interchangeably, leading to confusion about their distinct functionalities. Understanding the differences between EHR and EMR is crucial for healthcare professionals and patients alike. This comprehensive guide aims to provide a detailed overview of EHR vs EMR, their unique attributes, and their impact on healthcare delivery.
What is an Electronic Health Record (EHR)?
An EHR is a digital version of a patient’s paper chart. It contains a patient’s medical history, diagnoses, medications, treatment plans, immunization dates, allergies, radiology images, and laboratory test results.
What is an Electronic Medical Record (EMR)?
An EMR is a digital version of a patient’s paper chart in a single healthcare organization. It contains the medical and treatment histories of patients within one practice.
Key Differences Between EHR and EMR:
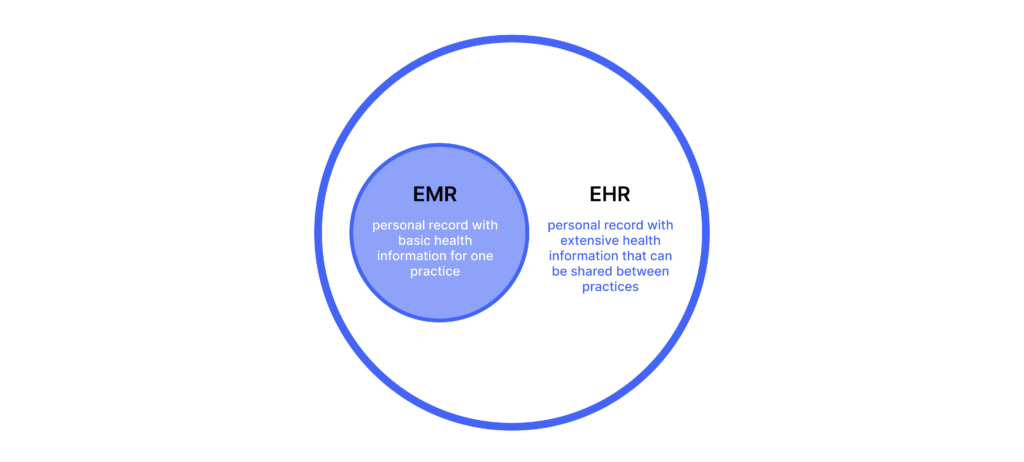
Understanding the key differences between Electronic Health Records (EHR) and Electronic Medical Records (EMR) is essential for healthcare professionals and patients navigating the increasingly digital landscape of medical information management. While EHRs encompass a patient’s comprehensive medical history across different healthcare settings, EMRs specifically focus on the medical and treatment histories within a single healthcare organization.
The distinction between these two systems impacts data accessibility, care coordination, and overall patient outcomes. By delving into the unique attributes of EHR and EMR, this guide aims to shed light on their distinct functionalities and their profound influence on the delivery of healthcare services.
Comparison of Features and Functions:
When comparing the features and functions of Electronic Health Records (EHR) and Electronic Medical Records (EMR), it is essential to recognize the distinct attributes that define their roles in healthcare information management. EHRs provide a comprehensive digital representation of a patient’s medical history, spanning across various healthcare settings. This includes diagnoses, medications, treatment plans, immunization records, allergies, radiology images, and laboratory results.
On the other hand, EMRs focus on the medical and treatment histories within a single healthcare organization. Understanding these differences is critical for healthcare professionals and patients navigating the evolving landscape of medical data management.
Integration and Implementation Challenges:
Integration and implementation challenges arise when healthcare organizations strive to seamlessly incorporate Electronic Health Records (EHR) and Electronic Medical Records (EMR) into their existing systems. The complexity of merging different data sources, ensuring interoperability, and maintaining data integrity poses significant hurdles.
Furthermore, training staff to effectively utilize these systems and ensuring compliance with regulatory standards present additional obstacles. Despite these challenges, successful integration and implementation of EHR and EMR can lead to enhanced data accessibility, streamlined care coordination, and improved patient outcomes. It is imperative for healthcare professionals to address these challenges proactively to harness the full potential of digital health records.
Impact on Healthcare Delivery and Patient Care:
The impact of Electronic Health Records (EHR) and Electronic Medical Records (EMR) on healthcare delivery and patient care is substantial and wide-ranging. EHRs, with their comprehensive digital representation of a patient’s medical history across various healthcare settings, have revolutionized the way healthcare professionals access and manage patient information. By providing a holistic view of a patient’s diagnoses, medications, treatment plans, immunization records, allergies, radiology images, and laboratory results, EHRs enable more informed decision-making and enhanced care coordination.
On the other hand, EMRs, focusing on medical and treatment histories within a single healthcare organization, streamline internal workflows and contribute to more efficient and personalized patient care within that specific practice. The integration and implementation of these digital records present challenges but hold the potential to significantly improve data accessibility, care coordination, and overall patient outcomes.
Conclusion
The distinction EHR vs EMR lies in their scope, functionality, and impact on healthcare delivery. While both systems have revolutionized the way patient information is managed, the comprehensive capabilities of EHR make it a vital tool for advancing population health management and improving patient outcomes. As healthcare continues to evolve, understanding the nuances of EHR and EMR is essential for driving innovation and enhancing the quality of care provided to patients.



